Individual selection of follow-up physiotherapy (simulators, muscle stimulators, Emsella electropulse therapy, BOS therapy), FemiLift fractional laser treatment, activated platelet therapy (PRP therapy) or surgical correction (plastic surgery with own tissues or using mesh implants) is carried out under clinical and instrumental ultrasound monitoring of the effectiveness of the chosen method.
Ultrasound of the pelvic floor muscles will be relevant for patients with complaints of urinary incontinence, feeling of a relaxed vagina, with decreased sexual sensations, pain in the perineum and vulva, after childbirth, to monitor previously performed surgical interventions on the perineum, evaluate the effectiveness of physiotherapy and for routine routine examination. As part of preventive anti-age therapy and in patients with connective tissue dysplasia, ultrasound diagnostics of the pelvic floor muscles allows timely detection of their thinning and correction on an outpatient basis, without resorting to surgery.| Assessment of urinary symptoms | Assessment of intestinal symptoms |
|
Urinary incontinence Recurrent UTIs Persistent dysuria |
Anal incontinence Difficult bowel movements |
| Symptoms of pelvic organ prolapse | Symptoms after pelvic floor surgery |
|
Implant ratings Slings Synthetic meshes for prolapse Fillers |
Vaginal discharge Bleeding Pelvic or vaginal pain |
|
Evaluation of cysts or formations of the vagina or perineum |
Assessment of childbirth-related symptoms |
| Dyspareunia |
Evaluation of the muscles that lift the anus Obstetric injury of the perineum and anal sphincter |
By default, the pelvic floor muscles are divided into 3 layers: outer, middle and inner. The outer layer is formed by the muscles involved in closing the entrance to the vagina and forming the tendon center of the perineum. The middle layer, or urogenital diaphragm, is the internal transverse perineal muscle through which the vagina and urethra pass.
And the deep layer is represented by powerful bundles of muscles that raise the anus, which surround the pelvic organs like a funnel, forming the pelvic diaphragm, also called the pelvic floor. The main components of the anus-lifting complex include the pubic-rectal, pubic-coccygeal and iliococcygeal muscles. The fibers that lift the anus converge behind the rectum, forming a lifting plate.
Pelvic floor muscles
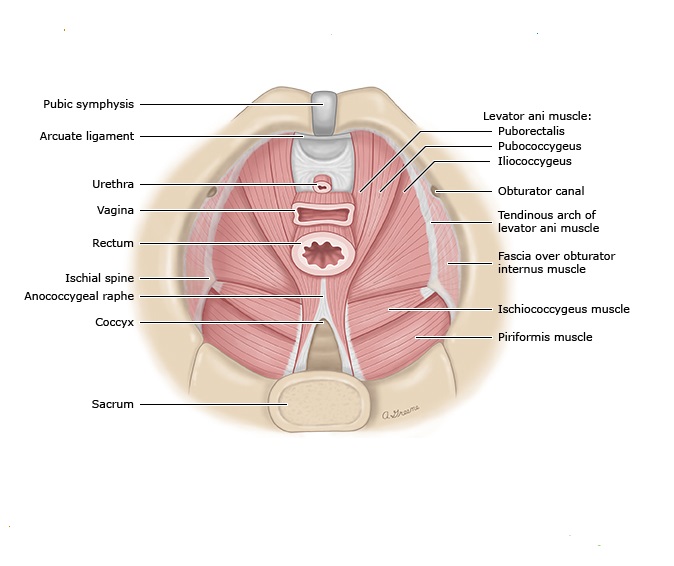
The basic tonic activity of the muscles that lift the anus keeps the minimum opening of the levator (the muscle that lifts the bone) closed, squeezing the urethra, vagina and rectum, forming a horizontal shelf on which the pelvic organs rest. Deficiency of any part of the anus-lifting muscle leads to weakening of the pelvic diaphragm and pelvic organ prolapse.
Trauma to the anus levators is common after vaginal delivery, with up to 24% of women having obvious muscle damage on postpartum ultrasound. Ruptures are repaired during the first year after delivery, but if a persistent defect persists, muscle failure develops with pain, impaired urinary retention, and the formation of recto- and cystocele. The symptoms may worsen with prolonged standing.
Studies have shown that women with pelvic organ prolapse experience a decrease in the number and function of muscle fibers, a higher rate of apoptosis, and disorganization of smooth muscle fibers.
Ultrasound of the pelvic floor muscles is a modern non-invasive technique that allows timely identification of asymptomatic patients requiring physiotherapy and to clarify the severity of abnormalities in women with symptoms who are preparing for surgical correction.
Who needs to have an ultrasound of the pelvic floor muscles and when?
We perform it at every ultrasound examination of the pelvic organs as part of a gynecological appointment for timely diagnosis and correction of pelvic floor muscle failure, as well as after childbirth to identify hidden muscle tears and select optimal options for physiotherapy and surgical recovery.








.webp)



.webp)



.webp)
