Removal of a cervical polyp
A cervical polyp is a pathological formation that develops on the wall of the cervical canal. At the EMC clinic, the diagnosis and removal of cervical polyps are performed by highly qualified gynecologists according to the most up-to-date international protocols.
General information
The cervix is the lower segment of the uterus that completes and connects its cavity with the vagina. The function of cervix is to protect the sterile uterine cavity from the penetration of bacteria from the vaginal environment. Usually, the cervix is tightly compressed and opens only during ovulation to allow sperm to enter, and during menstruation to evacuate spotting.
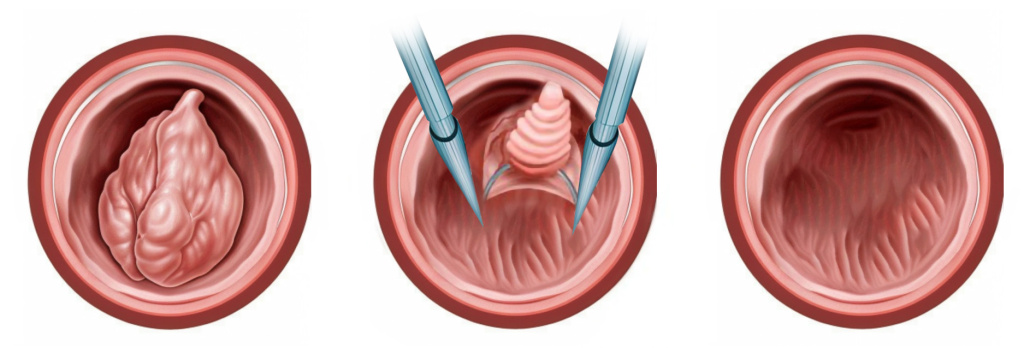
Normally, the cervix has a smooth pink surface. However, sometimes it forms tree-like outgrowths of connective tissue on a wide base or on a leg. These are polyps, formations that are quite often found in women aged 30-50 years and in the postmenopausal period.
Cervical canal polyps are the second most common pathology (after endometrial polyps) detected during gynecological examinations. Benign neoplasms of the cervix are detected in 2-5% of women. Malignancy is possible, but occurs in less than 0.1–1.5% of cases.
Patients often confuse the polyps of the cervix and endometrium, which form in the uterine cavity. Unlike endometrial neoplasms, cervical canal polyps are less likely to be accompanied by symptoms and are much less likely to become malignant. However, just as with the detection of endometrial pathology, a woman is shown an in-depth examination and treatment to eliminate the risk of complications.
Reasons
The causes of polyps in the lower part of the uterus have not yet been fully clarified. Risk factors include:
- Hormonal changes. Some studies suggest a link between polyposis and fluctuations in female sex hormones (estrogen), which explains the high prevalence of the pathology in premenopausal women.
- Damage to the mucous membrane. Polyps are more likely to develop after operations on the cervix (curettage procedure, abortions, obstetric manipulations), or in patients who had ruptures of the cervix during delivery.
- Infectious processes. Diseases such as colpitis, vulvovaginitis, cervicitis, sexually transmitted infections, and others can contribute to the development of polyps.
- Multiple pregnancies. Polyps are more often found in patients with a history of two or more pregnancies. However, in about 10% of cases, pathology is detected in women who have not given birth.
- Somatic diseases. The pathology is more often noted in patients with diabetes mellitus or obesity.
- Lifestyle factors. Chronic stress and lack of sleep, early onset of sexual activity, frequent change of sexual partners, etc. increase the risk.
Symptoms
In many women, cervical polyps do not make themselves felt by any manifestations and are detected by chance, at a preventive appointment or when dealing with other complaints. However, sometimes a neoplasm can be suspected by the following symptoms:
- A small amount of blood that is released after vaginal sex due to polyp injury.
- Menstrual cycle disorders. Discharge becomes very abundant, and sometimes abnormal uterine bleeding occurs outside of menstruation or after menopause.
- Pathological discharge. The polyp provokes the development of an infectious process and inflammation, which can lead to the appearance of white spots with an admixture of pus.
- Infertility. Sometimes the neoplasm closes the lumen of the cervical canal, preventing the penetration of sperm into the uterus.
Diagnostics
During the examination in the mirrors, the gynecologist can detect the polyp visually, especially if it is large and located in the outer part of the cervical canal. However, instrumental methods are used for accurate diagnosis
- Ultrasound. Transvaginal ultrasound helps determine the nature and localization of neoplasms of the reproductive system. However, small growths can be similar to normal structures, so their detection requires extensive medical experience.
- Colposcopy. Examination of the cervix with a large magnification makes it possible to detect the smallest tissue changes. At the same time, the doctor can conduct specialized tests with staining preparations that will differentiate the polyp in the outer part of the cervix with other pathological formations.
- Hysteroscopy. The diagnostic procedure is performed when it is necessary to examine the inside of the cervical canal and differentiate with an endometrial polyp. Hysteroscopy is an invasive procedure, so anesthesia is required. For diagnostic purposes, hysteroscopy can be performed at an outpatient appointment (office hysteroscopy) with local anesthesia. However, if a more extensive operation is required, including the removal of large polyps, diagnosis and treatment are performed under general anesthesia.
Treatment of polyps
If polyps have been identified according to the results of the preliminary examination, it is recommended to remove them. Without surgery, the probability of malignant degeneration of polypous formations is quite low, but it still exists. Conservative therapy cannot help in this case.
Usually, the removal of polyps is performed during therapeutic and diagnostic hysteroscopy. The operation is performed under general anesthesia, so the patient will need to undergo standard tests for surgical treatment (hospital complex, ECG, blood and urine tests). As a rule, treatment is carried out on the 6th-10th day of the menstrual cycle.
Before the operation, the patient will need to refrain from sexual intercourse, douching and the use of tampons, and also exclude meals a few hours before the hysteroscopy.

In the EMC clinic, hysteroscopy is performed using ultrathin optics with a diameter of 3-5mm, which does not require dilation of the cervical canal. Such a tool ensures rapid recovery, reduces the risk of injury and complications, even in unborn patients.
Removal of the polyp is performed through the surgical channel of the instrument. The surgeon precisely cuts the neoplasm with the help of miniature instruments that are inserted into the canal. After manipulation, the wound is cauterized, and the resulting biological material is necessarily subject to histological examination to identify abnormal cells.
In the first days after the procedure, there may be slight pain in the lower abdomen and slight spotting. Drug therapy (antibiotics, painkillers) may be prescribed. A protective regime is recommended for the patient during recovery: it is necessary to avoid bathing in open reservoirs and swimming in pools, visiting saunas, using tampons, and sexual intercourse .
At the EMC clinic, the treatment of polyps and other gynecological pathologies is conducted by experienced doctors according to the most up-to-date protocols. Make an appointment for a consultation by phone +7 495 933-66-55.
Make an appointment for a consultation and we will contact you for more details
Why the EMC
The first and only clinic in Russia, created in the image of the world's leading clinics
EMC is a multidisciplinary center offering patients a high level of medical services and a personalized approach
Worldwide recognition and awards
 Learn more
Learn more
Worldwide recognition and awards
 Certificates and licenses
Certificates and licenses



.webp)








.webp)

.webp)