Radiosurgery is a method of radiation therapy in which large doses of ionizing radiation are applied to the tumor, accuracy is very important when using this treatment method, from which the dose is applied to the target in order to avoid damage to the surrounding tissues. The use of radiosurgery as a method of treating malignant tumors began in the 1960s with the use of radiosurgery in the treatment of brain tumors. And the use of this treatment method for extracranial neoplasms dates back to the 1990s. Today, radiosurgery is one of the most important methods of treating malignant tumors of both the brain and the entire body, in some cases replacing completely surgical treatment. Radiosurgical treatment of lung tumors began in 1991 at Karolinska University (Sweden), and then it began to be used in Japan, the United States and Europe. To date, this treatment method is very promising in patients with the first stage of non-small cell lung cancer, as well as with single lung metastases.
Radiosurgery is a method of radiation therapy in which large doses of ionizing radiation are applied to the tumor, accuracy is very important when using this treatment method, from which the dose is applied to the target in order to avoid damage to the surrounding tissues. The use of radiosurgery as a method of treating malignant tumors began in the 1960s with the use of radiosurgery in the treatment of brain tumors. And the use of this treatment method for extracranial neoplasms dates back to the 1990s. Today, radiosurgery is one of the most important methods of treating malignant tumors of both the brain and the entire body, in some cases replacing completely surgical treatment. Radiosurgical treatment of lung tumors began in 1991 at Karolinska University (Sweden), and then it began to be used in Japan, the United States and Europe. To date, this treatment method is very promising in patients with the first stage of non-small cell lung cancer, as well as with single lung metastases.
Lung cancer currently occupies one of the leading positions in the statistics of deaths from neoplasms worldwide. In Russia, the incidence of lung cancer in the structure of malignant diseases in men is 17.8%, among women only 3.8%, while 60,000 people die annually. Timely and rational therapy can increase the five-year survival rate by 40-50%. With the development of diagnostic methods, the definition of lung cancer in the early stages is becoming more accessible. Today, surgery remains the standard of treatment for non-small cell lung cancer in the first stage of the disease, however, radiosurgery as a treatment method for such patients is a very worthy alternative, as studies show.
Historically, a group of patients over the age of 65 often did not receive the necessary treatment. This is due to the fact that surgical treatment in this group of patients increases the risk of death due to the presence of various concomitant diseases. Until 2000, radiation therapy with classical fractionation was mainly used in the treatment of lung cancer, and this is a long course of treatment, which is not always convenient for patients. On the contrary, when using radiosurgery, the treatment time is minimal, and excellent local control of the disease is achieved – these are important arguments in favor of choosing this treatment method.
Until 2000, radiosurgical treatment for non-small cell lung cancer was used mainly in patients who cannot undergo surgical treatment, namely: 1) in patients with stage 3 of the disease as part of complex therapy and 2) inoperable patients with stages 1-2 of the disease who have severe concomitant pathology. All other patients underwent surgical treatment more often in the amount of lobectomy or wedge-shaped resection.
After some time, studies appeared in Japan, the United States, and the United Kingdom, the results of which indicated that the overall survival in patients receiving radiosurgical treatment, despite a potentially worse prognosis, was the same as in patients after surgical treatment.
Analysis of research results conducted by Grills et al.(2010), Crabtree et al (2010), Verstegen et al (2013), Shirvani et al. (2014), Mohles et al. (2015) based on various statistical analysis methods (population analysis, data analysis based on propensity score, retrospective analysis) showed that the use of radiosurgery made it possible to achieve 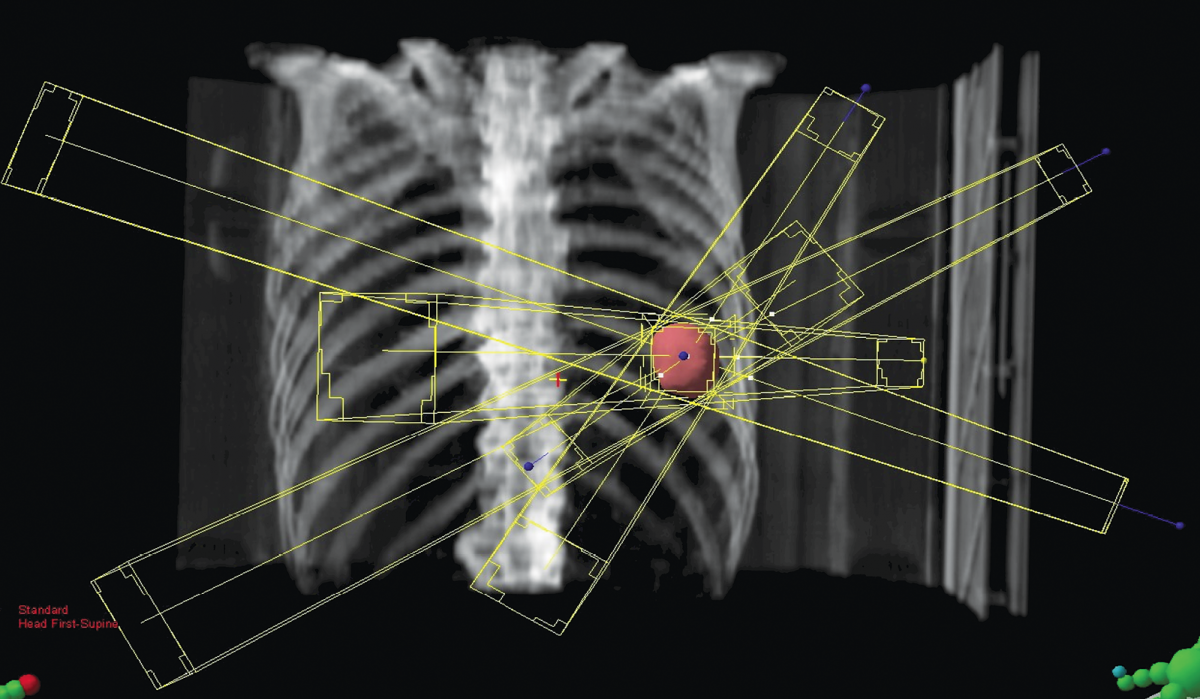 achieving better local disease control and surgery-comparable overall survival.
achieving better local disease control and surgery-comparable overall survival.
This served as the basis for conducting three randomized phase 3 trials: ROSEL, STARS, and ACOZOG Z4099 to compare the effectiveness of SBRT and surgical treatment in operable patients with stage 1 non-small cell lung cancer. These studies were soon stopped prematurely due to the low rate of patient recruitment.
The final analysis of the results of the Phase 3 STARS and ROSEL studies included 58 patients: 31 of them were in the stereotactic radiosurgery group, 27 were in the surgical treatment group. The median follow-up was 40.2 months. 6 patients died in the surgical treatment group, and only one in the radiotherapy group. The 3-year overall survival rate was 95% in the radiotherapy group and 79% in the lobectomy group.The 3-year disease-free survival rate between the groups was practically the same – 86% and 80% for stereotactic radiosurgery and surgery, respectively.Grade 3 and 4 complications were observed in 10% of patients in the SBRT group and 44% in the surgical treatment group, respiratory disorders in 6% in the SBRT group and 15% in the surgical treatment group, lung infection developed in 7% of patients in the surgery group and none in the the SBRT group.
Presenting these data in a report at the RUSSCO Congress on lung cancer treatment, Nidal Salima, Head of the EMC Radiotherapy Center and Chief Freelance Radiotherapy Specialist in Moscow, noted:"The aim of the research was to show that radiotherapy can be an alternative to surgical treatment in patients with early-stage lung cancer, but in fact it turned out that radiotherapy surpassed surgical treatment in a number of indicators."
In January 2018, the Journal of Clinical Oncology published data from a new meta-analysis comparing mortality rates after SBRT and surgical treatment in patients with early-stage lung cancer. The analysis included an extensive group of patients treated from 2004 to 2013: 76,623 patients after surgical treatment and 8,216 patients after SBRT. The analysis showed that the difference in 30-day and 90-day mortality increased in proportion to the age of the patients. The older the patients were, the higher the mortality rate after surgical treatment. The maximum advantages of SBRT over surgery were noted in patients over 70 years of age. This allowed the authors to conclude that it is necessary to make a joint informed decision regarding patients who are suitable for both types of treatment.
Currently, several randomized trials are being conducted in the world at the same time to compare the effectiveness of SBRT and surgical treatment of stage 1 lung cancer in operable patients.
The decision to include a patient in a surgical treatment group or SBRT is made by an interdisciplinary group that includes a surgeon, a radiotherapist, a pulmonologist, and a clinical research nurse. Experts hope that this approach will avoid the bias inherent in previous studies, when patients initially had an appointment with a surgeon.
"Stereotactic radiotherapy is well tolerated by patients and shows high efficacy. In the near future, it may become the standard of treatment for operable patients with stage I non—small cell lung cancer, becoming a full-fledged alternative to surgical treatment," said Nidal Salim.
The EMC Radiation Therapy Center in Moscow has accumulated extensive experience in using the SBRT technique in the treatment of lung tumors.In three years of operation the oncology clinic has completely cured 100 patients, and the survival rate for patients with early-stage lung cancer is 95%. Treatment is carried out on an outpatient basis without interrupting work and a habitual lifestyle.
Questions and answers
.webp)




















.webp)








.webp)

.webp)