Content
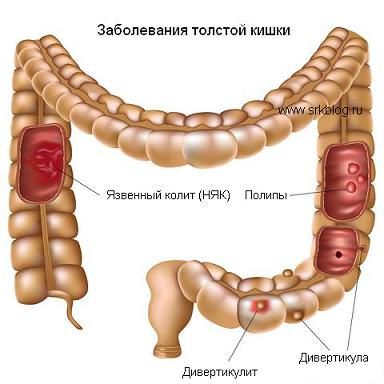 It is a chronic inflammatory disease of the mucous membrane of the colon (colon and rectum) with the formation of multiple ulcers. This disease is one of the most serious problems for gastroenterologists and coloproctologists: in terms of severity, complication rate and mortality rate, it occupies one of the leading places among diseases of the gastrointestinal tract worldwide. The first peak of morbidity occurs at the most active working age — 18-25 years, the second peak – after 55. The disease is chronic and requires constant medication and frequent inpatient treatment.
It is a chronic inflammatory disease of the mucous membrane of the colon (colon and rectum) with the formation of multiple ulcers. This disease is one of the most serious problems for gastroenterologists and coloproctologists: in terms of severity, complication rate and mortality rate, it occupies one of the leading places among diseases of the gastrointestinal tract worldwide. The first peak of morbidity occurs at the most active working age — 18-25 years, the second peak – after 55. The disease is chronic and requires constant medication and frequent inpatient treatment.Why does ulcerative colitis develop?
The causes of this disease have not yet been definitively clarified. It is assumed that exposure to a variety of adverse factors leads to an excessive inflammatory response that occurs due to hereditary or acquired disorders in the mechanisms of regulation of the immune system. As a result, non-infectious inflammation of the intestinal mucosa develops.
There is a genetic predisposition to the development of this disease: if a first-line relative (mother, father, sister, brother) suffers from ulcerative colitis, the risk of developing the disease is very high.
Symptoms of ulcerative colitis
Intestinal damage in the initial stages can be limited only to the rectum, gradually spreading throughout the colon. The main manifestations of ulcerative colitis are frequent loose stools up to 25 times a day, with an admixture of blood and mucus, cramps and abdominal pain, weight loss. More than half of the patients have extra—intestinal manifestations of the disease: damage to the joints, eyes (iridocyclitis — inflammation of the iris, uveitis—inflammation of the vascular membrane of the eye), skin (erythema nodosum — inflammatory lesion of the skin and subcutaneous vessels, pyoderma - purulent skin lesion), oral cavity (aphthous stomatitis — inflammation of the oral mucosa with the formation of erosions), the liver. In some cases, these manifestations of the disease may precede the appearance of intestinal symptoms.
How is ulcerative colitis diagnosed?
 Diagnosis is based on the results of endoscopic (intraluminal) examination of the intestine — colonoscopy and histological examination of intestinal tissue samples. Colonoscopy allows you to visually assess the condition of the colon almost throughout its entire length (up to 2 meters), detect signs of inflammation (characteristic appearance of the mucous membrane), pseudopolyps (polypous changes in the intestinal mucosa under the influence of inflammation) and, if necessary, take pieces of the mucous membrane for histological analysis.
Diagnosis is based on the results of endoscopic (intraluminal) examination of the intestine — colonoscopy and histological examination of intestinal tissue samples. Colonoscopy allows you to visually assess the condition of the colon almost throughout its entire length (up to 2 meters), detect signs of inflammation (characteristic appearance of the mucous membrane), pseudopolyps (polypous changes in the intestinal mucosa under the influence of inflammation) and, if necessary, take pieces of the mucous membrane for histological analysis.In some cases, if it is impossible for the patient to perform a colonoscopy, an irrigography is performed – an X–ray examination of the colon using a contrast agent, which makes it possible to detect defects in the mucous membrane - erosions and ulcers, pseudopolyps and altered, deformed areas of the intestine as a result of the inflammatory process.
In the initial diagnosis of ulcerative colitis, it is necessary to exclude the infectious nature of the disease (feces are analyzed for pathogens of bacterial and parasitic intestinal infections), as well as to determine the level of fecal calprotectin — this indicator characterizes the intensity of inflammation in the intestine.
Treatment of ulcerative colitis
Drug treatment in the acute phase of the disease is carried out with hormonal anti–inflammatory drugs, supportive therapy with non-hormonal anti-inflammatory drugs and immunosuppressants (drugs that suppress the pathological immune response), including the so-called biological drugs — monoclonal antibodies. In most patients, modern conservative therapy makes it possible to control the course of ulcerative colitis, however, according to the literature and our own data, up to 30% of patients require surgical treatment due to the ineffectiveness/intolerance of drug therapy or due to the development of complications, including a high risk of developing colon cancer, the more likely it is. the longer the duration of the disease. If a child suffering from ulcerative colitis has a slowdown in physical development due to prolonged hormone intake, surgical treatment is the method of choice. Severe intestinal complications — intestinal bleeding, toxic dilation (dilation) of the colon, perforation (rupture) of the intestine — are indications for emergency surgery.
Previously, surgery consisted of removing the entire colon (colon and rectum — coloproctectomy) with the formation of a permanent ileostomy. The operation completely eliminates the disease and the risk of developing cancer in the colon or rectum, but is accompanied by the need for lifelong use of colostomy bags (special bags for collecting secretions from the intestine).
Modern reconstructive plastic surgery consists in removing the colon and rectum to the anal canal and forming a reservoir (J-pouch) from the small intestine, which takes over the functions of the rectum. The reservoir accumulates stool, due to this, defecation becomes controlled, the frequency decreases to 4-6 per day. Surgical intervention frees the patient from long-term treatment with medications with pronounced side effects, the operation eliminates the further development of colitis, and the risk of developing bowel cancer is minimized.
Each UC surgery has its advantages and disadvantages, and the method of surgical intervention is discussed individually in each case. The EMC Coloproctology Clinic successfully performs all types of operations for UC, including total coloproctectomy with the formation of a small intestinal reservoir.
Was this information helpful?
Questions and answers
Ask a Question





.webp)







.webp)

.webp)
.webp)





.webp)


