About 152 thousand women die from ovarian cancer every year. At the same time, if the disease was detected at an early stage, the five–year survival rate of patients – and this indicator, in fact, means a complete recovery - reaches 94%. But ovarian cancer is extremely difficult to diagnose and requires an oncologist to pay attention to indirect details. And the accuracy of diagnosis and the effectiveness of therapy directly depend on the doctor's experience.
Ovarian cancer, according to the International Agency for Research on Cancer, is diagnosed annually in about 239,000 women worldwide. If you compare this indicator with the detectability of other malignant neoplasms, it may seem that this is not a disease that requires a woman to be more alert. Thus, the incidence of breast cancer exceeds the figures for ovarian tumors by seven times. But the insidiousness of this cancer becomes obvious if we analyze the statistics of mortality from cancer. The number of deaths from the most common female cancer (breast cancer) and ovarian tumors does not differ so much at all: mortality rates differ by 3.7 times. Another example: ovarian tumors are diagnosed with approximately the same frequency as thyroid malignancies, but ovarian cancer accounts for 4.3% of the overall mortality rate from all cancers, while thyroid cancer accounts for only 0.8%.
I must say, the high mortality rate from this disease is a global trend. The American Cancer Society ranks ovarian cancer fifth in the structure of mortality from all cancers in women, and first among cancers of the reproductive organs. There are similar trends in Russia: according to the Russian National Research Center. According to Blokhina, ovarian tumors are among the five most common diseases that lead to the death of women aged 40 to 69 years. The alarming statistics are primarily due to the asymptomatic course of the disease. This makes early diagnosis difficult, when doctors can offer the most effective and organ-preserving treatment. As a result, approximately 75-80% of ovarian tumors are diagnosed at stage III-IV.
"Ovarian cancer has many non-specific symptoms that women themselves and, often, doctors do not pay enough attention to. The patient may change her weight, appetite, tone, and discharge, but these symptoms are quite common and are characteristic of other diseases," explains the head of the EMC Women's Health CenterVladimir Nosov. – Even women with stage three ovarian cancer go to an oncogynecologist, on average, six months after the first complaints appear. All this time, patients are being "chased" by gastroenterologists, psychiatrists, for example, with irritable bowel syndrome."
Ovarian cancer diagnosis
The situation is further complicated by the lack of an accurate, specific diagnostic method that meets all the requirements of oncologists. The most common method is ultrasound examination, which can "miss" changes in the ovary. Specialists have similar claims, albeit to a lesser extent, to CT and MRI.
The practice of diagnosing ovarian cancer using the CA-125 cancer marker in Russian medical institutions causes nothing but skepticism among Western school specialists: the CA-125 marker was invented and certified for a very specific purpose – tracking the effectiveness of treatment in patients with already diagnosed ovarian cancer. "In half of cases, patients with stage I and II ovarian cancer the level of CA-125 is absolutely normal, while a lot of benign diseases – fibroids, endometriosis, cysts, and even diarrhea can increase this indicator significantly," explains Vladimir Nosov, who studies and works at hospitals at Yale (Yale-New Haven Medical Center) and California (UCLA-Cedars Sinai Medical Center) universities.
Currently, all efforts of specialists are focused on the search for new diagnostic methods that can detect ovarian cancer at an early stage. In the meantime, given the lack of highly effective diagnostic methods, the oncologist's experience, attentiveness, alertness, and ability to combine many indirect factors play almost a key role. "It may seem that the doctor is asking general questions, wondering if the patient's tone has changed over the past six months, if there has been any pain, if the stool has changed. But our doctors are focused on forming the overall picture – individually, these issues are not specific, but together they allow us to "catch" cancer," says Vladimir Nosov.
EMC has developed specialized cancer prevention programs, while the list of tests in the Check-up takes into account the age of patients (groups 18-39 years old, 40-49 years old, 50 years and older). Regular examinations increase the chances of detecting precancerous or cancerous changes in the early stages, when the probability of cure is maximum, clinicians emphasize.
Another feature of the disease is its ability to be inherited. Approximately 10-20% of women with this disease have a genetic predisposition to ovarian and breast cancer: if they have the BRCA1 mutation, they are 54% and 85% likely to develop a tumor, respectively. An even more depressing fact is that in this case, cancer affects the youngest women. In the practice of Russian oncologists, widespread testing of women for the BRCA1/2 mutation has not yet been widely used, clinicians regret to note. "After all, a woman has a mammary gland, which in this case is also under fire, and besides, her children, regardless of gender, are 50% likely to get this mutation," explains Vladimir Nosov.
Modern technologies for the treatment of ovarian cancer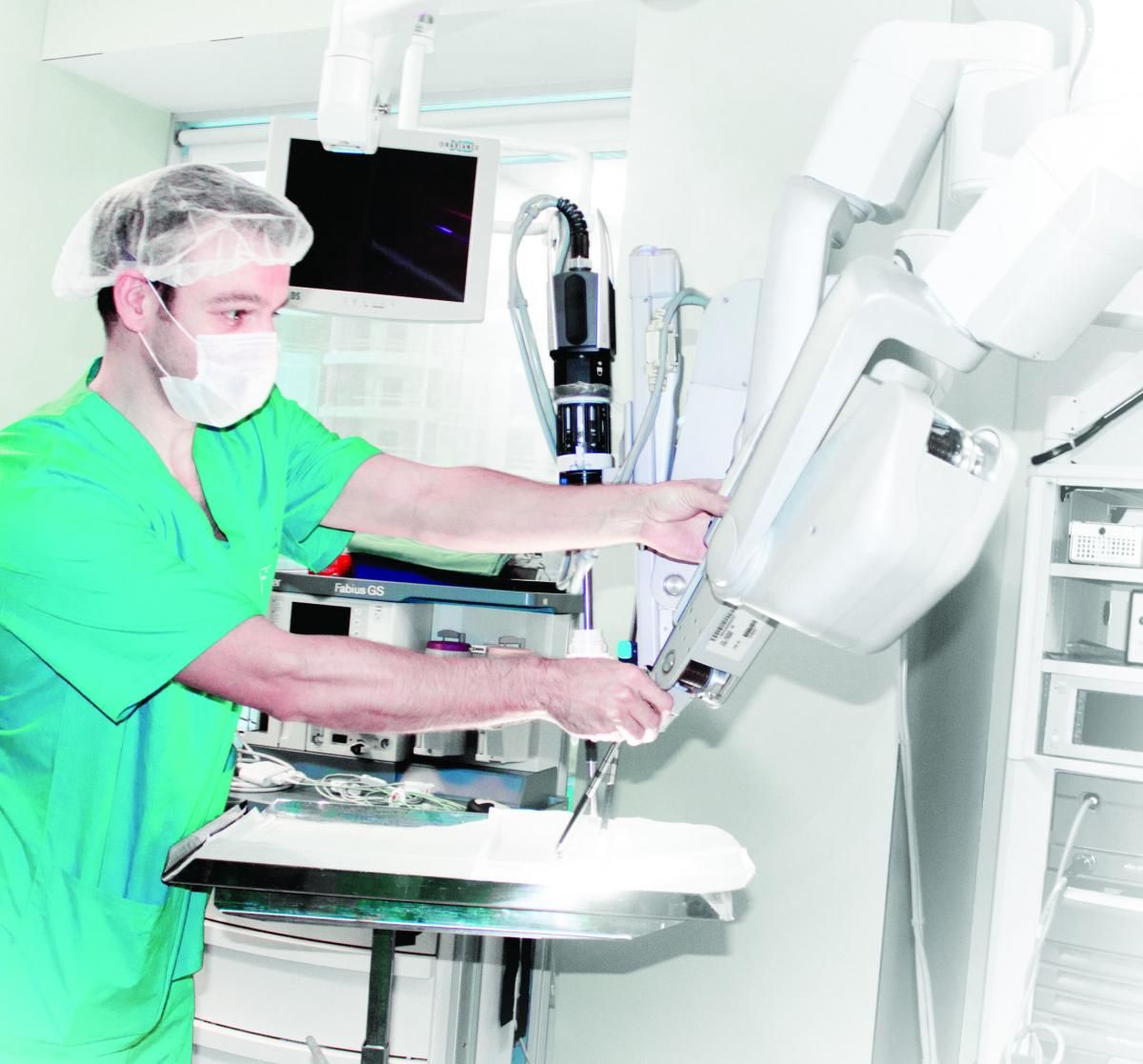 Do not forget about the correct modern treatment of the disease. If doctors manage to detect a tumor in the early stages, when it has not yet spread beyond the ovary, but if the tumor process has spread, there is no need to talk about organ-preserving treatment. Ovarian cancer very often affects the organs of the abdominal cavity, invading the spleen, intestines, other organs and lymph nodes of the retroperitoneal cavity. In this case, the probability of optimal cytoreduction becomes particularly relevant. This term means that after surgery, not a single lesion larger than 1 cm remains in the abdominal cavity. This approach requires the oncologist to be extremely careful and focused, but it is practically the main factor influencing the future prognosis. "Patients with optimal cytoreduction have a five–year survival rate of 35-40%, and women with a 2 cm lesion have a 5% survival rate," notes Vladimir Nosov.Organ–preserving operations can be performed to remove only the affected ovary, while preserving the uterus and fallopian tubes. The advantages of such treatment are obvious: a woman does not lose her hormonal function, she still has the opportunity to have a child (or use IVF), and she does not have to deal with premature menopause. But the prevalence of such minimally invasive surgeries is not high for two reasons: the percentage of localized tumors detected is not high – only 15-20%, another deterrent factor is medical conservatism. Clinics where such operations are put on stream can literally be counted on the fingers.
Do not forget about the correct modern treatment of the disease. If doctors manage to detect a tumor in the early stages, when it has not yet spread beyond the ovary, but if the tumor process has spread, there is no need to talk about organ-preserving treatment. Ovarian cancer very often affects the organs of the abdominal cavity, invading the spleen, intestines, other organs and lymph nodes of the retroperitoneal cavity. In this case, the probability of optimal cytoreduction becomes particularly relevant. This term means that after surgery, not a single lesion larger than 1 cm remains in the abdominal cavity. This approach requires the oncologist to be extremely careful and focused, but it is practically the main factor influencing the future prognosis. "Patients with optimal cytoreduction have a five–year survival rate of 35-40%, and women with a 2 cm lesion have a 5% survival rate," notes Vladimir Nosov.Organ–preserving operations can be performed to remove only the affected ovary, while preserving the uterus and fallopian tubes. The advantages of such treatment are obvious: a woman does not lose her hormonal function, she still has the opportunity to have a child (or use IVF), and she does not have to deal with premature menopause. But the prevalence of such minimally invasive surgeries is not high for two reasons: the percentage of localized tumors detected is not high – only 15-20%, another deterrent factor is medical conservatism. Clinics where such operations are put on stream can literally be counted on the fingers.








.webp)



.webp)



.webp)
