Ankylosing spondylitis - what is it?
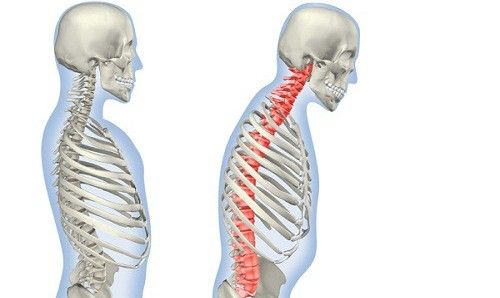
Ankylosing spondylitis is a systemic inflammatory disease, a type of spondyloarthritis that affects the joints, spine, and entheses (attachment points of ligaments and tendons to bones). The difference between the disease and other spondyloarthritis is that the vertebrae are ankylosed (fused) together, as a result, the spine can turn into a single bone and deform. The quality of life in this disease is significantly reduced. The second serious complication of Ankylosing spondylitis is damage to the hip joints, up to complete loss of mobility and disability.
Why does this disease occur?
The exact cause of the disease is unknown. According to one hypothesis, individual intestinal microbes can trigger pathological inflammation in the prostheses and joints. For the appearance of the disease, it is not enough for a certain infection to enter the body, a certain state of the body's immune system is necessary, in which self-sustaining inflammation is possible. The scientifically proven risk factors for developing ankylosing spondylitis are heredity and smoking.
Symptoms
Ankylosing spondylitis usually begins to develop at a young age. The most common symptom of Ankylosing spondylitis is back pain. This pain has a number of characteristic features (the so-called "inflammatory back pain"). It increases with prolonged immobility, including during night sleep, and decreases with physical activity. Pain of an inflammatory nature is often accompanied by a feeling of stiffness, especially in the morning when the patient wakes up. The presence of this symptom is a reason to immediately consult a specialist to clarify the diagnosis. Young people often have pain in the area of the calcaneus or the attachment points of the Achilles tendons.
The disease most often begins with sacroiliitis, which is manifested by pain in the lower back (lumbar region). But in some cases, the patient may feel pain in the neck or at the level of the thoracic spine. In the later stages, movement restrictions appear, and in particularly severe cases, a "supplicant's pose" is formed.
Patients often report pain, limited mobility, and swelling in peripheral joints, such as the shoulder, hip, small joints of the hands and feet, and the temporomandibular joint.
The disease can also cause extra–articular manifestations, such as damage to organs such as the heart, kidneys, and eyes. The latter is most common and is manifested by uveitis (pain, photophobia, redness of the eye).
Among the associated conditions are the presence of psoriasis, inflammatory bowel diseases, intestinal or genitourinary infections.
Depending on the area where the inflammation develops, the central and peripheral forms of the disease are distinguished.
Diagnostics
The diagnosis is confirmed using instrumental and laboratory diagnostic methods. X-ray and MRI are used as complementary methods in the diagnosis of ankylosing spondylitis. Ultrasound examinations or MRI of the hands and feet often make it possible to effectively detect enthesitis (inflammatory lesions of the entheses).
Laboratory diagnostics play a significant role. 90% of patients with ankylosing spondylitis are carriers of the HLA B-27 gene. It is a genetically determined leukocyte antigen that is associated with the possibility of developing an autoinflammatory reaction. However, the presence of HLA B-27 does not mean the development of the disease, this gene only indicates an increased risk of ankylosing spondylitis.
Early diagnosis is the key to successful treatment of Ankylosing spondylitis, but it is not easy to recognize the disease. A lot depends on the qualifications of a rheumatologist.
Treatment of Ankylosing spondylitis
Medical treatment
The treatment is based on nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, diclofenac, naproxen, nimesulide, etoricoxib, ketoprofen, aceclofenac, meloxicam, etc. They are able to inhibit ankylosing of the spine, reduce the inflammatory response, improve the prognosis of the disease, increase the volume of movements and at the same time can be used as painkillers. Drugs block the self-sustaining autoinflammatory process and block the mechanism of the disease. Patients with peripheral involvement who have arthritis are recommended to take basic anti-inflammatory drugs (sulfasalazine, leflunomide, methotrexate). If there is no effect from taking nonsteroidal anti-inflammatory drugs, patients are prescribed genetically engineered drugs from the group of tumor necrosis factor inhibitors
Surgical treatment
Surgical treatment may be required to correct conditions associated with complications of the disease, such as severe spinal deformities, vertebral fractures, hip joint destruction, and heart damage.
Physical Therapy
Physiotherapy methods can be used to relieve pain: massage, acupuncture, etc. methods. Their disadvantage is that they do not have a long-term sustainable effect. Physiotherapy is not included in the official recommendations for the treatment of Ankylosing spondylitis.
Physical therapy
Regular physical exercise in addition to basic therapy helps to maintain joint mobility. Exercises to strengthen the back muscles are especially recommended.
Prevention
The causes of the disease have not been reliably established, so no special prevention has been developed.
General recommendations may include maintaining an active lifestyle, while trying to avoid spinal and joint injuries, abstaining from smoking, and eating a Mediterranean diet..
EMC diagnostics and treatment
Due to a wide range of diagnostic methods and modern technologies, most patients with this disease manage to achieve a good effect in treatment. The European Medical Center (Moscow) provides comprehensive care according to protocols adopted by international rheumatology organizations (ASAS, EULAR, ACR). For patients who cannot come to the clinic, it is possible to arrange an absentee consultation.
Why the EMC
The first and only clinic in Russia, created in the image of the world's leading clinics
EMC is a multidisciplinary center offering patients a high level of medical services and a personalized approach
Worldwide recognition and awards
 Learn more
Learn more
Worldwide recognition and awards
 Certificates and licenses
Certificates and licenses
Make an appointment for a consultation
Specify your contacts and we will contact you to clarify the details
Reviews
and new products of the EMC


.webp)



.webp)


.webp)


.webp)


.webp)
.webp)

.webp)