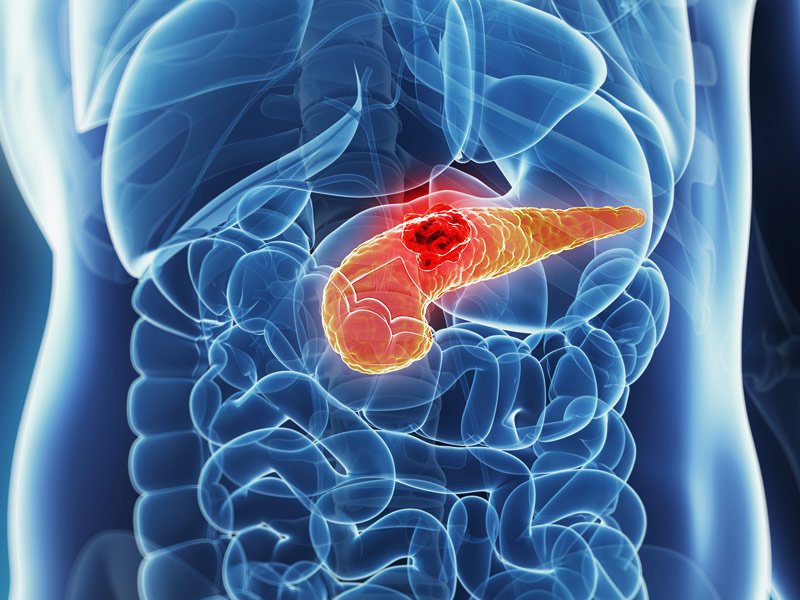
Pancreatic cancer
 The pancreas is an organ of the digestive system that performs two main functions:
The pancreas is an organ of the digestive system that performs two main functions:
-
production of enzymes for the digestion of fats, proteins and carbohydrates;
-
insulin production.
In 80% of cases, cancer develops in the head of the pancreas. There are several types of pancreatic cancer. The most common type is ductal adenocarcinoma, which develops from the glandular epithelium lining the surface of the bile ducts. It accounts for about 95% of all types of pancreatic cancer.
Less common types:
-
Cystadenocarcinoma (cystic tumors)
-
Acinar cell carcinomas;
-
Neuroendocrine tumors;
-
Lymphomas
Risk factors for pancreatic cancer:
-
Old age. In most cases, pancreatic cancer develops after the age of 65.
-
Smoking. 3 out of 10 cases of pancreatic cancer in developed countries are associated with smoking.
-
Diet. A diet containing large amounts of red meat, as well as processed meat (ham, sausages, bacon, etc.), increases the risk of developing the disease. Regular consumption of sugar and fatty foods and a lack of fruits and vegetables in the diet are also associated with an increased risk of pancreatic cancer.
-
Alcohol. Moderate alcohol consumption does not affect the development of pancreatic cancer. But drinking alcohol in large quantities can lead to cancer, especially in smokers.
-
Body weight and physical activity.
According to the results of some studies, overweight (obesity) and a sedentary lifestyle can contribute to the development of pancreatic cancer. Presumably, 1 out of 8 cases of morbidity is associated with obesity.
Certain diseases and conditions may also increase the risk of pancreatic cancer:
-
Chronic pancreatitis.People who suffer from chronic pancreatitis for a long time may have an increased risk of developing pancreatic cancer. The risk is higher in patients with hereditary pancreatitis.
-
Diabetes.Diabetes increases the risk of developing pancreatic cancer. At the same time, it should be understood that diabetes mellitus is common, and the vast majority of patients do not develop pancreatic cancer.
-
Genetic predisposition. About 5-10 out of every 100 cases (5-10%) may be caused by a hereditary gene anomaly. If two or more family members on the same line have pancreatic cancer, their direct relatives are at risk. People with the BRCA2 gene mutation, who are at risk for breast cancer, as well as patients with Lynch syndrome/HCV (hereditary non-polypous colorectal cancer) also have a higher risk of developing pancreatic cancer. Hereditary diseases such as familial atypical nevi and melanoma syndrome (FAMMM syndrome) and Peitz–Jaegers syndrome are also associated with a high risk of pancreatic cancer.
Symptoms of pancreatic cancer
Pancreatic cancer can be asymptomatic for a long time.
The most common symptoms are upper abdominal pain, weight loss, and jaundice.
The pain usually starts in the upper abdomen and can radiate to the back. The pain can be temporary or permanent, and usually increases in the prone position.
Jaundice develops if a tumor located in the head of the pancreas blocks the bile duct. Bile accumulates in the body, causing symptoms such as yellowing of the skin and whites of the eyes, itching of the skin, darkening of urine. Please note that jaundice can be caused by other diseases.
Other possible symptoms of pancreatic cancer:
-
loss of appetite;
-
dyspepsia;
-
feeling of fullness after eating;
-
nausea;
-
diarrhea
-
fatigue
-
depression.
Most often, the above symptoms are associated with other diseases, and a doctor's consultation is necessary to clarify the diagnosis.
Diagnostics
Diagnosis of pancreatic cancer at an early stage is difficult, as its symptoms coincide with the manifestations of other more common diseases.
The examination of the patient usually begins with a visit to the doctor, who conducts an examination, prescribes a urine test for bile enzymes, a general and biochemical blood test.
-
Instrumental examination methods – ultrasound, endoscopic ultrasound, CT, MRI make it possible to clarify the localization of the tumor and assess the extent of its spread to neighboring organs. In some cases, ERCP (endoscopic retrograde cholangiopancreatography), a method combining X–ray and endoscopic examination, is performed to eliminate obstruction of the bile ducts or to take a biopsy.
-
Biopsy – obtaining a small area of organ tissue for examination under a microscope. If pancreatic cancer is suspected, a biopsy is performed during endoscopic ultrasound or ERCP. In some cases, a puncture biopsy is performed under ultrasound or CT control.
-
Blood tests (cancer marker).In most cases of pancreatic cancer, an increased content of the CA 19-9 antigen is found in the blood. Nevertheless, elevated levels of CA 19-9 in the blood can occur in other diseases, and a normal level of this substance is not a guarantee that there is no cancer. Measuring the level of CA 19-9 is not the method of choice for primary diagnosis, but it is of great importance for monitoring the effectiveness of treatment and follow-up.
Pancreatic cancer treatment
Surgical treatment
The most effective treatment for pancreatic cancer at an early stage is surgical treatment.
Before surgery, it is important to discuss with your doctor all the advantages and risks of surgical treatment. Depending on the location of the tumor and the prevalence of the process, the following operations can be performed:
-
Gastropancreatoduodenatal resection (according to Whipple) with preservation of the gatekeeper. It involves the removal of the head of the pancreas, duodenum, choledochus, gallbladder and surrounding lymph nodes. It is commonly used in the treatment of pancreatic glans.
-
Gastropancreatoduodenatal resection (according to Whipple) is the same as the previous operation, but with the removal of the lower part of the stomach;
-
Pancreatectomy is the total removal of the pancreas
-
Distal pancreatectomy – removal of the tail and body of the pancreas.
After resection or removal of the pancreas, the patient is prescribed medications containing digestive enzymes and insulin.
Symptomatic interventions
In some cases, when total removal of the tumor is impossible, partial resection is performed to reduce the size of the tumor as palliative therapy, as well as surgical interventions to relieve the symptoms of the disease:
-
Duodenal bypass or stenting;
-
Duodenal bypass or stenting;
-
Percutaneous transhepatic cholangiography
Chemotherapy and radiation therapy
Chemotherapeutic treatment for pancreatic cancer is used:
-
After surgery to reduce the risk of recurrence (adjuvant chemotherapy)
-
For inoperable tumors to reduce size and control the disease
-
To relieve the symptoms of the disease;
In some cases, combined chemoradiotherapy is recommended.
Why the EMC
The first and only clinic in Russia, created in the image of the world's leading clinics
EMC is a multidisciplinary center offering patients a high level of medical services and a personalized approach
Worldwide recognition and awards
 Learn more
Learn more
Worldwide recognition and awards
 Certificates and licenses
Certificates and licenses
Make an appointment for a consultation
Specify your contacts and we will contact you to clarify the details
Reviews
and new products of the EMC

.webp)